Revenue leakage is one of the biggest headaches for healthcare providers. Every small documentation error, delayed filing, missing modifier, or insurance mismatch adds up and affects the overall financial performance of a practice. Many organisations underestimate how much these gaps impact their cash flow until they start seeing repeated claim denials or growing accounts receivable days. According to recent studies, a fully integrated EHR-plus-billing system can reduce claim denials by as much as 39%, dramatically improving cash flow for practices.
The shift toward integrated digital systems is not just a technology decision anymore. It is becoming core to financial sustainability. That’s where stronger EHR-driven workflows make a measurable difference. When clinical and billing teams share the same source of truth, the entire payment journey becomes smoother, cleaner, and far more efficient. Here’s what we’ll cover: what EHR in medical billing really means, why it’s increasingly essential, how to implement it successfully, the key advantages, and ways it strengthens the payment system.
What Is EHR in Medical Billing?
EHR in medical billing means the electronic health record systems, combined with billing and revenue cycle management systems. In these systems, clinical information like data, notes and treatment are not separated into different clinical databases, but are allowed to flow into billing workflows. This integration eliminates duplicate data entry, increasing the accuracy of coding and streamlining the process of claims generation.
In simpler terms, instead of having clinicians’ care documentation in one system and then passing the data to the billing teams in different systems, one EHR is used for both care documentation and management of the financial workflows. This process is the foundation for minimising and speeding up errors in the payment life cycle.
Why You Need EHR in Medical Billing Software?
1. Reducing Errors at the Source
One of the biggest causes of claim denials is improper or incomplete data, patient data discrepancies, wrong codes, missing modifiers, and other similar factors. Healthcare EHR systems with integrated validation can catch many of these issues early, during patient data entry, for example, in real time during patient registration, where it provides eligibility checks and validation of the demographic information.
2. Faster, Cleaner Claims
When an EHR medical billing application powers the billing workflow, then there is a close coupling of clinical documentation and clinical coding. Automated coding and scrubbers can validate claims before submission. This results in higher first-pass acceptance rates.
3. Better Revenue Capture & Cash Flow
When claims are accepted on the first submission, then there are no outstanding appeals, re-works or denials of the claims and thus, which results in more rapid cash flow and predictable cash flow. Integrated electronic health record technology also eases the operational workload on billing staff.
4. Compliance & Audit Readiness
Since systems are integrated and work on structured clinical data, every billing action is accompanied by documentation. This documentation eases the compliance burden and provides more defence for audits while also providing a documented risk mitigation.
How to Successfully Implement EHR in Medical Billing?
Implementing a system that combines electronic medical record systems for hospitals (or clinics) with billing is nontrivial. Here’s a roadmap to do it successfully:

-
Assessment & Planning
Organisations determine their unique billing issues and workflow deficiencies devoid of an orderly evaluation and strategising phase. Both billing and clinical teams should be included early because their collaboration will determine the efficiency of the new workflow for the EHR. This is also the stage when teams must determine if they require bespoke construction as opposed to a pre-packaged EHR and billing solution.
-
Choose the Right Platform
The following phase is to determine the optimal solution. Healthcare teams should assess the different types of healthcare software and other EHR systems in healthcare, based on their capacity to sustain effective revenue cycle management combined with automated coding opportunities, claim scrubbing, and eligibility verification. Interoperability is always of the utmost importance; due to this, the selected solution must have the capacity to integrate seamlessly with payer systems, clearinghouses, and data analytic applications to ensure the absence of data silos.
-
Data Migration & Integration
Organisations move to the stage of data migration and integration. This is the stage where the patient records, claimant information, and historical claims data are transported to the new system. At this stage, the seamless movement of data between clinical documentation and the billing system is critical to ensure that information flow is both correct and consistent throughout the system.
-
Training & Change Management
Once implementation is complete, training and change management activities start. New workflows are introduced to every team that has contact with any patient or billing data. As confusion alleviates, a role-based interface streamlines operations for different teams. A pilot phase is essential so that the organisation can detect and address issues before wide-scale deployment.
-
Testing and Optimisation
Testing and Optimisation. Over and over the process goes. The scrubbing engines, the automated alerts, and code suggestions must be tested against actual cases. Denial rates and days in AR are useful performance indicators to measure improvement. When the system matures, stakeholders can employ predictive analytics to assess risks and spotlight potentially denyable claims.
-
Continuous Improvement & Scaling
Then there is the final phase, which is continuous improvement and scaling. With dashboards and leveraging the benefits of healthcare BI software in place, healthcare organisations can monitor and respond to fluctuating patterns and trends, deny claims audits, and continuously improve their workflows. The system is then ready to scale across departments or even entire facilities when it is reliable and proves to be financially beneficial.
Want to integrate EHR into your medical billing workflow with a reliable tech partner?
What are the Advantages of EHR-Integrated Billing?
Let’s break down the major advantages in more detail:
-
Reduced Denials
Integrated systems offer validation in real-time, code automation, and claim scrubbers that assist in preventing the most common errors that are common and often result in denials. With better data flowing from clinical notes to billing workflows, teams are able to submit more precise claims and sidestep the endless back and forth with payers. This also allows for a more dependable billing process and lessens the operational burden on employees.
-
Improved Accuracy & Compliance
Users can document and map every diagnosis, procedure, and note the appropriate codes alongside integrated electronic health record technology. This ensures that everything is accurate. This level of documentation is what helps mitigate risk from audits, support compliance, and guarantee that regulatory checks are in place.
-
Shorter Payment Cycles
There is faster reimbursement because the claims are of better quality. Also, as the billing that is driven by an Electronic Health Record can significantly decrease the payment cycle. With the help of the integrated EHR, users can fix many errors in real-time eligibility checks as claims get generated.
-
Lower Administrative Burden
The need for manual re-keying, follow-up, and appeals is less. This also helps operational costs and allows billing teams to concentrate on strategic tasks. Thus, opposed to the rework that is generated from the automation.
How EHR in Medical Billing Improves the Payment System?
Now, let’s dive deeper into ways EHR in medical billing improves the payment system, specifically.
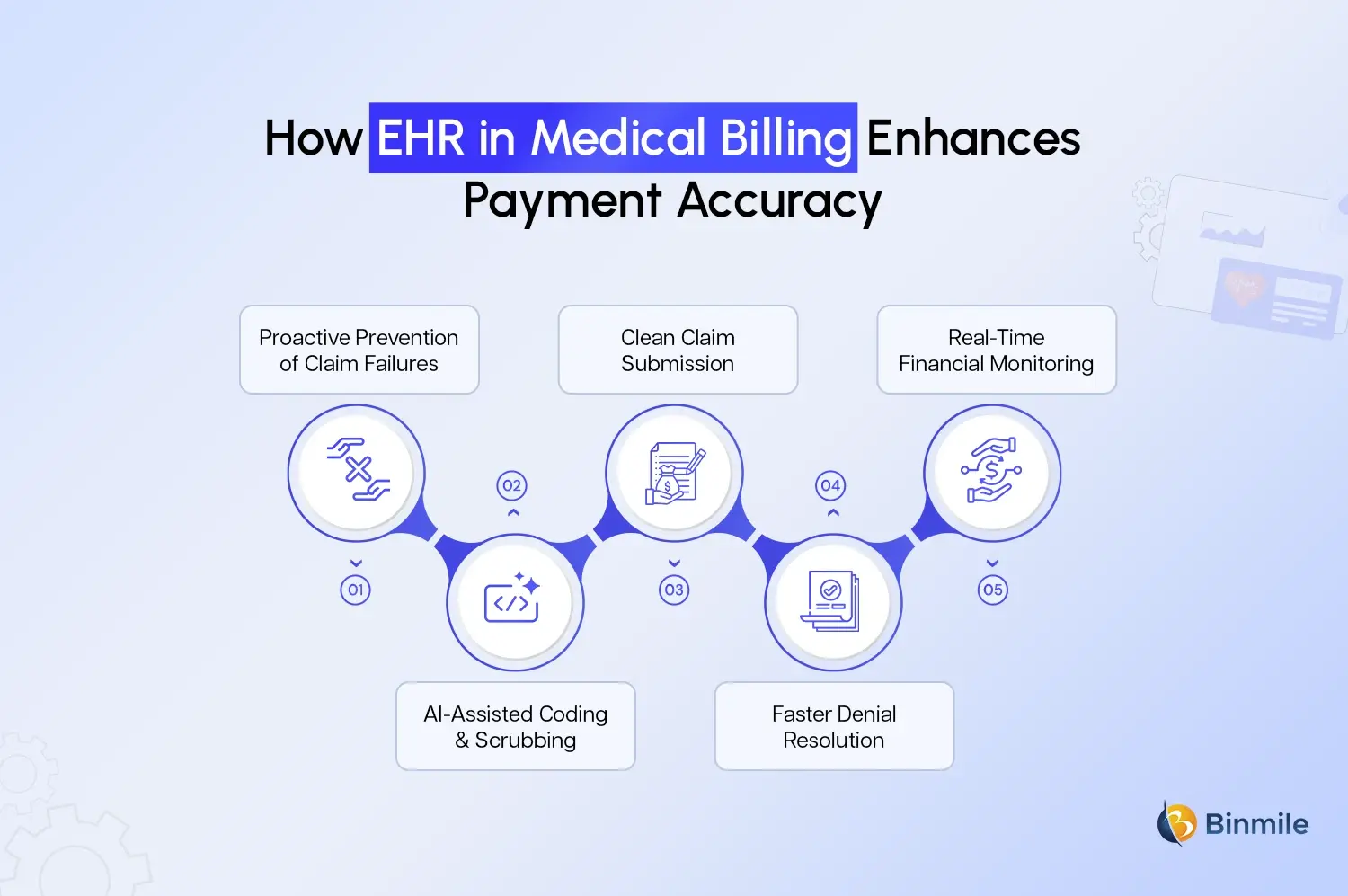
1. Proactive Prevention of Claim Failures
Through the incorporation of real-time eligibility verification, the system detects payer mismatches, ineligible plans or lapsed coverage during patient intake. Thus, it reduces the creation of claims with incorrect insurance data, additionally leading to fewer front-end denials.
2. AI-Assisted Coding & Scrubbing
The latest EHR medical billing software products include AI-enhanced coding engines that review clinical notes. Additionally, propose an optimal coding solution and AI medical transcription software in healthcare, which is more accurate than any manual coding action. These systems also automatically scrub claims to identify missing or inconsistent data, which prevents the submission of high-risk claims.
3. Clean Claim Submission
With clinical data seamlessly passing into billing with no duplication, mismatched demographics errors and omitted modifiers automatically reduced. These factors, combined with scrubbing features of claims, increase the submission of clean claims with high first-pass acceptance rates.
4. Faster Denial Resolution
When a claim is denied, the integrated system can help determine the primary factor (eligibility, coding, or missing documentation). Additionally, automate aspects of the appeal workflow. With cleaner data and less manual intervention, denial management becomes more expedient, accurate, and simpler to complete for billing teams.
5. Real-Time Financial Monitoring
Because all billing data lives in the same system as clinical data, financial and operational teams can monitor key metrics like denial rates, average AR days, and payment lag in real-time. This insight helps leaders act swiftly on trends and optimise workflows.
Looking to optimise billing, claims, and payment cycles with seamless EHR implementation?
How Binmile Can Help You Build or Optimise Such a System
Improving the link between EHR workflows and billing requires clean integrations and a good understanding of healthcare processes. Binmile supports providers with custom software integration services, helping connect EHR platforms with billing engines, clearinghouses, and payer systems in a secure and streamlined way.
For teams that require a more tailored setup, their experience as a custom healthcare app development company enables them to design modules that align with real-world clinical and billing workflows. They also integrate AI medical transcription software in healthcare, which turns clinical notes into accurate billing data and reduces manual effort. To strengthen financial visibility, Binmile helps implement healthcare BI software, giving teams clearer insights into denials, AR days, and claim performance.
With secure data flows, better documentation, and smooth EHR-billing coordination, Binmile helps healthcare providers reduce errors, cut down denials, and improve payment outcomes without disrupting daily operations.
Frequently Asked Questions
AI assists with automation in the coding process (suggesting CPT/ICD codes), in claim scrubbing (identifying discrepancies), and in the process of denials management (estimating risk, automating the drafting of appeals). These increase the speed of reimbursement and decrease errors.
EHR systems increase the speed of reimbursement by integrating clinical documentation with billing and ensuring data accuracy, less manual entry, credentialing, and support for clean claim submissions.
The EHR integrated billing systems contain organised clinical and financial records. Each step is captured in a way that can be documented, traced, and audited, which lessens the chances of fraud, audit failure, or non-compliance with regulations.
Electronic health records enhance documentation and the standardisation of data collection. Validation rules in the system improve consistency, coding engines that suggest appropriate codes, and eligibility checks that prevent mismatches between the patient and the insurance. All of this results in fewer errors related to billing.
Some of the most common negative impacts of the implementation of EHR systems are high implementation costs, complexity of data migration, change management (staff training), system interoperability, and maintaining continuous optimisation.