Healthcare Revenue Cycle Management Software is not just another tool for hospitals and clinics. It sits at the heart of financial stability for healthcare providers by automating complex billing and administrative processes that once consumed time, money, and staff energy. According to industry estimates, the global market for revenue cycle management solutions is poised to increase significantly through this decade, reflecting how essential these systems have become to healthcare financial performance.
Many healthcare leaders now recognize that without scalable, integrated systems managing revenue flow from patient registration to final payment, their operations risk inefficiencies, claim denials, and revenue leakage. In this blog, we explore how to develop scalable Revenue Cycle Management Software tailored for healthcare, what key features it must include, how modern technologies like AI in healthcare improve performance, crucial compliance considerations, software and hardware decisions, development challenges, and real-world best practices for successful deployment.
What is Revenue Cycle Management in Healthcare
Revenue Cycle Management in Healthcare refers to the end-to-end process that a provider uses to capture, manage, and collect patient service revenue. It starts when a patient schedules or checks in for a service, and it ends when the provider receives full payment. This process involves multiple steps: eligibility verification, charge capture, claim submission, payment posting, denial management, and patient collections.
The primary goal of an RCM platform is to maximize cash flow, minimize errors and denials, improve financial transparency, and ensure a seamless interaction between clinical care and financial operations.
Why Scalable RCM Software Matters
Healthcare providers vary vastly in size and complexity, from single-clinic practices to multi-facility hospital groups. Flexible RCM software for healthcare will need to grow with the entity, process increasing data loads, and changing regulatory requirements, and interoperate with other systems like Electronic Health Records (EHRs).
Here are the important reasons scalability matters:
A growth-ready architecture ensures that Healthcare Revenue Cycle Management software can handle increasing patient volumes and higher claim loads without affecting system performance. As an organization grows, its RCM software should improve with it and not require large renovations. Additional modular features (e.g., advanced analytics, denial prediction) improve flexibility by allowing systems to provide more on-demand capabilities when an organization is ready to utilize them.
Multi-facility support helps centralize revenue cycle workflows across multiple locations, giving organizations better control and consistency in operations. Together, these capabilities future-proof the system, enabling healthcare providers to adapt to evolving care models like telehealth billing and value-based care without disruption.
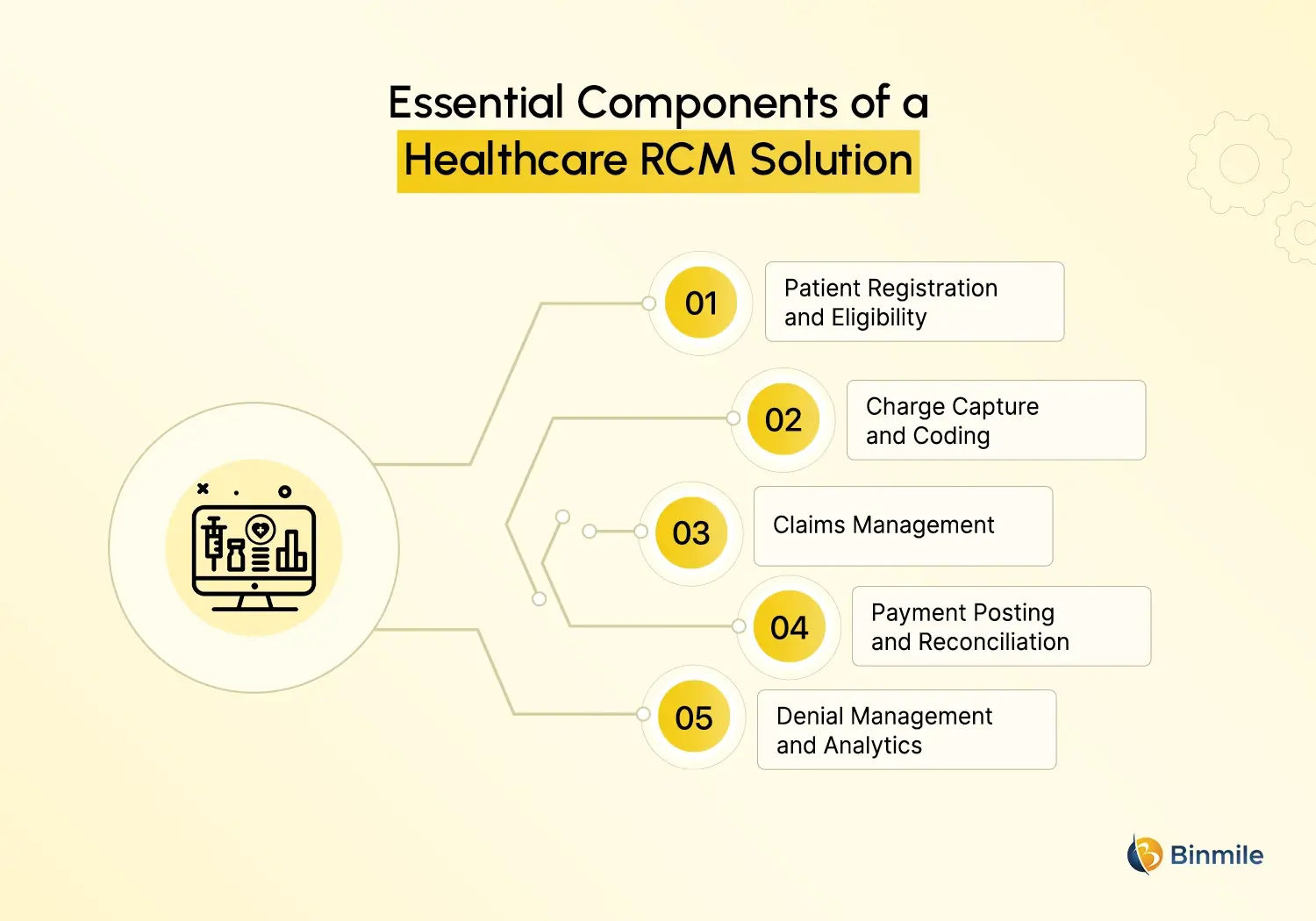
What are the Core Components of a Healthcare RCM Solution
To build an effective healthcare RCM solution, you must design with a detailed understanding of the revenue cycle and its challenges. Below is a breakdown of essential components.
-
Patient Registration and Eligibility
The revenue cycle begins with patient registration. Systems need to document patient demographic information and insurance details while doing a real-time insurance verification. Systems that have real-time alerts for fields that are left blank and for inconsistent answers help identify errors early so that claim rejections and payment delays later in the healthcare revenue cycle management process can be avoided.
-
Charge Capture and Coding
Charge capture and coding make sure that the services rendered are billed appropriately. Automating charge entry based on clinical documentation helps reduce the need for manual entry. Consistency with standard coding systems like ICD and CPT is maintained, and system coding guides and validation rules help reduce the chances for denials.
-
Claims Management
The goal of claims management is to focus on collecting and submitting claims that are complete, accurate, and ready to be processed by the payers. With clearinghouses, claim submission is automated for maximum efficiency. Claims get scrubbed to capture and fix errors before submitting the claims. They can instantly stop a claim from being processed and edit information in order to add a payor that is more appropriate.
-
Payment Posting and Reconciliation
This component is for payments received from the insurance and the patients. Automated processes for posting payments minimize the work and errors associated with manual posting. This is the core feature of the healthcare compliance software. Reconciliation tools aid in clearing discrepancies between amounts billed and paid. Financial dashboards update in real-time to show available cash and overall revenue performance.
-
Denial Management and Analytics
Managing and analyzing denials is crucial for maintaining revenue integrity. Systems in place for the capture of the reason for the denial should aid in cause-and-effect analysis, and system-driven appeals, when possible, this should automate to streamline the process. Advanced analytics dashboards capture recurring issues and lost revenue to help streamline the process and ultimately improve revenue forecasting.
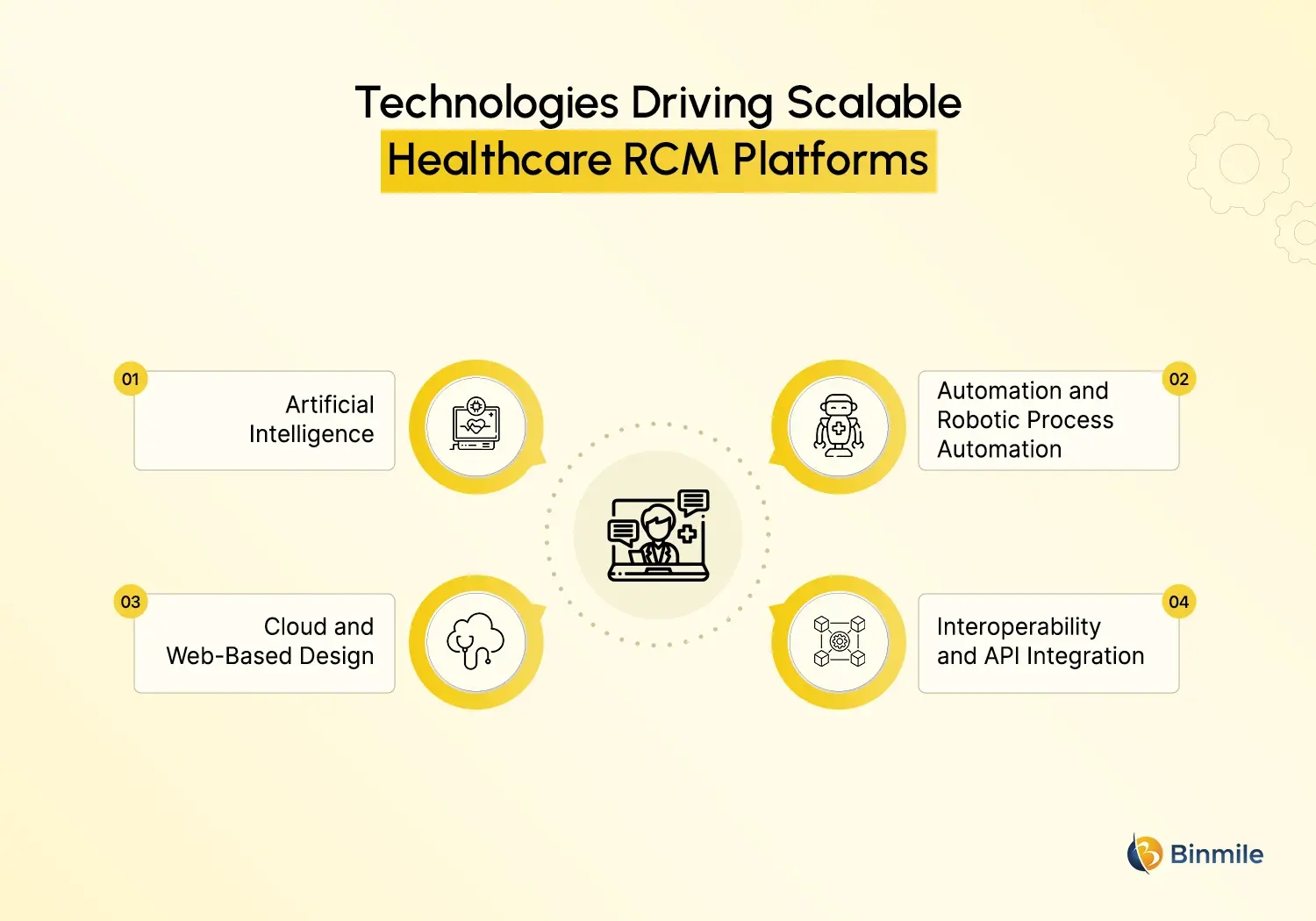
What are the Key Technologies Powering Scalable RCM Platforms
Modern healthcare RCM software is not static. It uses evolving technologies to increase speed, accuracy, and intelligence.
-
Artificial Intelligence
AI in healthcare positively impacts RCM processes. Healthcare software modernization with Intelligent systems, for example, recognizes patterns for possible claim denials and recommends edits before submissions. Also, advanced analytics support organizations in predicting revenue cycles, which helps in financial planning.
-
Automation and Robotic Process Automation
When tasks are automated, such as insurance checking, claim submissions, and posting payments, the work and mistakes involved are diminished. Not only are cycle times reduced, but billing staff are able to focus more on exception handling and communication with patients.
-
Cloud and Web-Based Design
Cloud systems offer better scalability, secure remote accessibility, and lower cost of ownership when compared to on-premises systems. Healthcare organizations utilizing RCM systems in the cloud experience fewer system updates, improved data consolidation, and enhanced disaster recovery.
-
Interoperability and API Integration
APIs help bridge gaps between RCM systems and others, like EHR, CRM, and payer portal systems. APIs provide real-time data exchanges, help eliminate data silos, and improve overall workflows, including mobile app development initiatives for billing access, patient payments, and reporting.
Struggling with claim denials and revenue leakage? Discover how bespoke RCM solutions can transform your financial operations today.

Designing for Compliance and Security
Healthcare is one of the most regulated industries, and healthcare management software must meet stringent standards.
-
HIPAA and GDPR Compliance
The financial and health records of patients are among the most sensitive data an organization can possess. In the U.S., the RCM systems must comply with HIPAA, and for any operations in Europe, the RCM systems must have GDPR compliance. Therefore, the RCM systems must have strong access controls, auditing, and encryption, as well as thorough logging.
-
Audit Trails and Secure Logging
Every action in a system should be recorded with an audit trail. This increases accountability and helps with compliance during audits and investigations.
-
Regular Compliance Updates
Software must be updated regularly to comply with new regulations, such as coding updates (ICD revisions) and new payer policies, to minimize the risk of claim denials and financial penalties.
Architecture Practices for Scalability
Building scalable healthcare software is no longer optional, especially for systems that manage critical financial workflows like revenue cycle management. The underlying architecture supports future growth, higher data volumes, and increasing user demand without requiring frequent or costly redesigns. A well-planned architecture, especially AI in patient care, ensures long-term stability while allowing the software to evolve as operational needs change.
A microservices-based approach plays a key role in achieving scalability. By breaking the RCM platform into independent services such as billing, claims processing, and analytics, each component can scale based on its own workload. This approach improves flexibility, simplifies updates, and reduces the risk of system-wide failures when changes are made to individual modules.
Horizontal scaling further strengthens system performance by distributing workloads across multiple servers instead of relying on a single machine. This improves reliability and ensures consistent performance during peak usage periods, such as high claim submission cycles. Alongside this, continuous performance monitoring is essential. Embedding tools that track system health, database efficiency, and user experience helps teams identify bottlenecks early and take corrective action before they impact revenue or operations.
Feature Comparison of Scalable vs Traditional RCM Platforms
| Feature | Traditional RCM | Scalable RCM Software |
|---|---|---|
| Deployment | On-premises | Cloud or Hybrid |
| Updates | Manual | Automated Updates |
| Integration | Limited | API-driven |
| AI/Automation | Minimal | Built-in |
| Scalability | Rigid | Elastic, on-demand |
| Analytics | Basic | Advanced dashboards |
| Cost Structure | High upfront | Subscription or pay-as-you-grow |
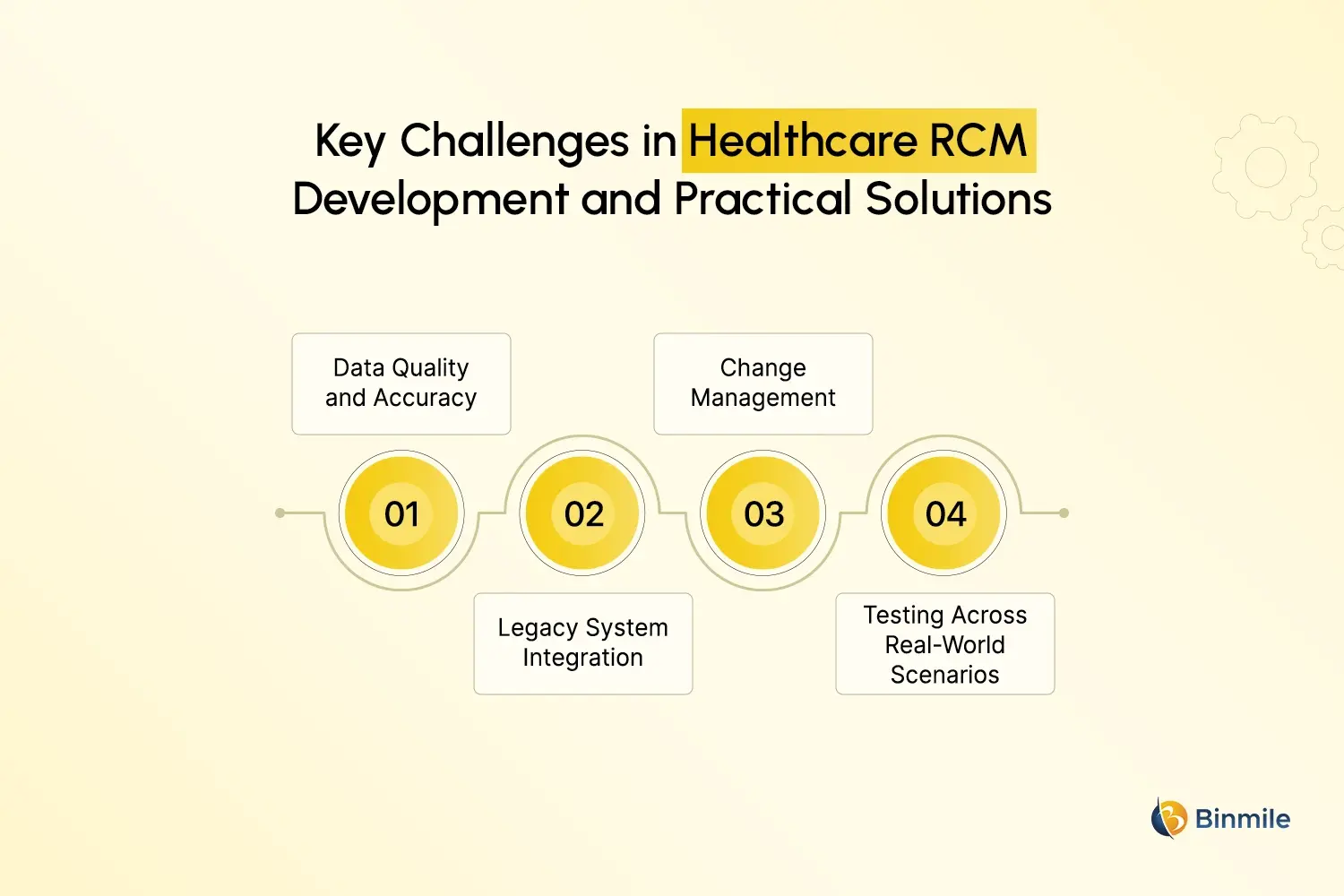
What are the Common Challenges in RCM Development and How to Overcome Them
-
Data Quality and Accuracy
Incorrect and inconsistent data lead to claim denials and slow cash collection. Build user-friendly data interfaces that validate and correct data entry at every step of the workflow.
-
Legacy System Integration
Many healthcare systems still use older technology. Design your integrations to include robust API connectors and middleware that link the old and new systems seamlessly.
-
Change Management
New solutions can be met with resistance. To help with the adoption of new systems, provide simple interfaces, complete training, and gradual implementations to users.
-
Testing Across Real-World Scenarios
Testing the software to ensure it meets expectations in real-life situations by evaluating and accounting for the claims based on different payers’ rules, claim types, and distinct circumstances.
Case Example: How Modern RCM Improves Financial Outcomes
Consider a midsize hospital that shifts to a scalable RCM platform. With real-time eligibility checks, automated claim scrubbing, and AI denial prediction, the organization reduces claim denials by double-digit percentages and cuts days in accounts receivable significantly. With faster revenue conversion and fewer manual rework tasks, billing teams can focus on high-value work.
Want to streamline your billing workflows with a custom RCM platform built for your healthcare organization?

How a Technology Partner Helps Build Scalable RCM Software
Developing advanced RCM software for healthcare requires deep expertise in both healthcare workflows and software engineering. A partner with experience in custom software development, healthcare web development, cost estimation, custom healthcare app development, and regulatory compliance can steer the project from concept to launch efficiently. They can help you select the right tech stack, design secure data handling processes, and integrate seamlessly with existing systems such as EHRs and payer networks. Combining domain knowledge with strong technical execution ensures your software delivers measurable improvements in financial performance while empowering staff with intuitive workflows.
This is where a partner like Binmile fits naturally into the process. By combining healthcare domain knowledge with scalable architecture design, robust engineering capabilities, and a strong focus on best revenue cycle management software practices, Binmile supports organizations in building healthcare RCM solutions that are reliable, compliant, and ready to grow. The result is software that improves financial performance, reduces operational friction, and empowers healthcare teams with intuitive, efficient revenue cycle workflows.
Frequently Asked Questions
RCM software automates billing and financial workflows, reduces manual errors, speeds up claim processing, improves cash collections, and increases revenue visibility across the entire revenue cycle in healthcare operations.
AI helps predict claim denials, automate coding, identify patterns in billing errors, and provide insights into revenue trends, resulting in faster reimbursements and fewer administrative delays.
Yes, scalable RCM platforms use APIs to connect with major EHR systems, enabling real-time data exchange, reducing data duplication, and streamlining clinical-to-financial workflows.
Healthcare RCM systems must comply with privacy and security standards, such as HIPAA for patient data protection and, where applicable, GDPR for global operations, including secure logging and encryption.
Development timelines vary based on features, integrations, and custom requirements, but typical projects range from several months to a year, including planning, design, development, testing, and deployment.